For anesthesiologists, new research is advancing the use of artificial intelligence (AI).
- Rating
- enable anesthesiologists
- unconscious medication
- anesthesiologists cautious
- anesthesiologists
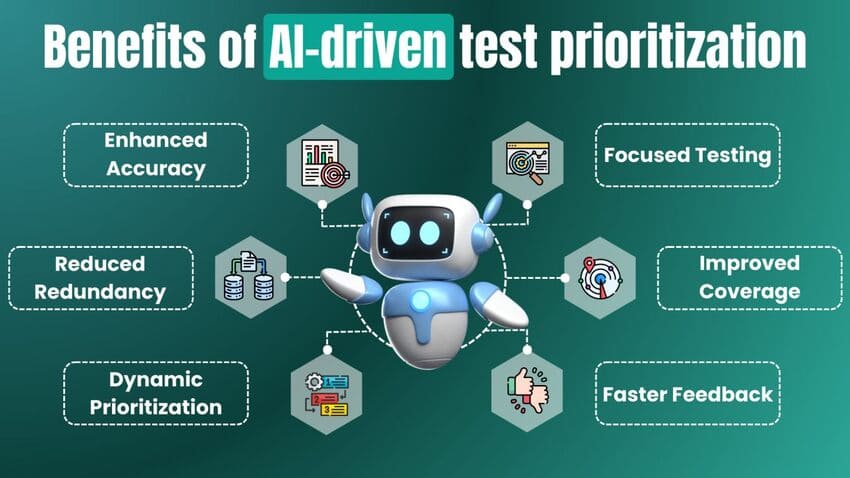
A team of neuroscientists, engineers, and doctors showed a machine learning algorithm for constantly automating the dosage of the anaesthetic medication propofol in a special issue of Artificial Intelligence in Medicine. With a deep reinforcement learning application, the neural networks of the software learned how to maintain unconsciousness while also critically evaluating the efficacy of its own actions. This algorithm outperformed more traditional software in sophisticated, physiology-based simulations of patients. When compared to actual anesthesiologists, it was very accurate in simulating what they would do in order to keep patients unconscious throughout nine genuine procedures.
Computers can now keep patients unconscious with less medication, thanks to algorithm advances, which frees anesthesiologists to focus on other tasks in the operating room, such as ensuring that patients are immobile, pain-free, physiologically stable, and getting enough oxygen. These are just a few of the many responsibilities anesthesiologists currently have in the operating room.
Schamberg, a former postdoc at MIT and the study's corresponding author, likened his objective to that of an airplane's auto-pilot, where the captain is always in the cockpit and constantly monitoring the system. It makes sense to automate the components of patient care that we understand well since anesthesiologists must concurrently monitor various aspects of a patient's physiological condition.
The algorithm's ability to assist optimise medicine dose might enhance patient care, according to senior author Emery N. Brown, a neuroscientist from MIT's Picower Institute for Learning and Memory and Institute for Medical Engineering and Science.
According to Brown, the Edward Hood Taplin Professor of Computational Neuroscience and Health Sciences & Technology at MIT, "Algorithms such as this one enable anesthesiologists to keep more cautious, near constant supervision over the patient throughout general anaesthesia.
Actor as well as critic
Using a machine learning method, researchers were able to develop a system that would learn how to dose propofol to keep a patient unconscious, but also how to do it in the most efficient manner possible. A "critic" and a "actor" were added to the software to assist the "actor" perform in a way that maximised the "rewards" provided by the programmer, and they were able to do this by using two neural networks. They trained the algorithm with three distinct incentives, for example: one punished just overdose, one questioned the provision of any dosage, and one placed no penalties at all on the system.
In all cases, they used simulations of real patients to train the algorithm using sophisticated models of both pharmacokinetics and pharmacodynamics, or how rapidly propofol dosages reach the important brain areas after administration. In the meanwhile, brain wave measurements accurately represented the extent of patient unconsciousness, just as they would in a real operating room. It is possible for both the actor and the critic to improve their performances for various types of patients by running hundreds of simulation rounds using a range of values for these situations.
The most successful incentive system was the "dose penalty" one, in which the critic questioned every dosage the actor administered, continuously chastising the actor to keep dosing to a sufficient minimum to maintain unconsciousness. The system sometimes dosed too much and sometimes dosed too little without any penalties. In comparison to the other value models and the usual software, the "dose penalty" model learnt faster and created less inaccuracy.
An experienced mentor
Schamberg and Badgeley put the "dose penalty" algorithm through its paces in the operating theatre by feeding it patient consciousness data obtained from actual instances. The algorithm's strengths and weaknesses were shown throughout the testing.
During most experiments, the algorithm's dose decisions closely matched those of the attending anesthesiologists after unconsciousness was caused and before it was no longer required. In contrast to the anesthesiologists (who all had plenty of other things to do), the algorithm changed dose every 20-30 minutes, as Badgeley observed.
The researchers admitted that the algorithm was not designed to induce unconsciousness in the first place. They stated that the programme doesn't know when surgery is finished on its own, but that's easy for the anesthesiologist to handle.
Leave a Reply
Your email address will not be published. Required fields are marked *